INTRODUCTION
The sensation of dyspnoea can be frightening and the words used to describe this subjective feeling such as breathlessness, suffocation, drowning and smothering can add to the anxiety of the person and their family/whanau. Dyspnoea may also be described as laboured breathing or air hunger.
DEFINITION
Dyspnoea is a subjective symptom that does not always fit with the physical signs. Studies have shown that what onlookers see as distressing, e.g. laboured and rapid breathing, may not be distressing for the person.
There are reported three paradigms of dyspnoea:
- A perceived increase in respiratory effort, to overcome a pulmonary load. Often seen in people with airway obstruction disease, anxiety or a large pulmonary effusion.
- Increase in the proportion of chest wall strength and respiratory muscles required to maintain homeostasis, the mechanism found in people with neuromuscular disease (MND) and cancer cachexia.
- An increase in respiratory demand due to exercise, sepsis, acidosis or hypoxemia.
ASSESSMENT
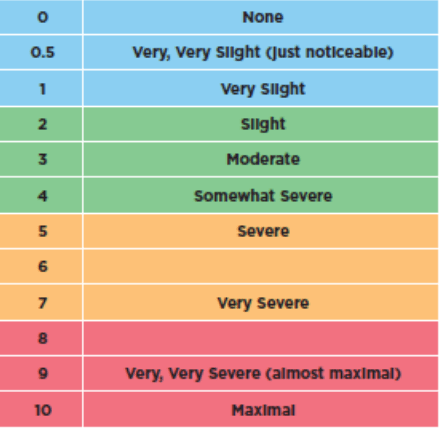
- As this is a subjective experience, the assessment where possible should be based on the person’s report, using a structured tool such as a visual analogue scale. Or by scoring the level of their own breathlessness from 0-10, 0 being no breathlessness to 10 being the most severe breathlessness ever experienced by the person.
- Signs of severe breathlessness include excessive use of accessory muscles, gasping breathing, arms fixed down onto the mattress and “pursed lip breathing”.
- In the unconscious person at the end of life the health care professional (HCP) will have to rely on physical clues such as tachyopnea (fast breathing), tachycardia (fast heart rate/pulse), sweating, grimacing, agitation and use of accessory muscles to identify dyspnoea.
MANAGEMENT
POSITIONING
- Being upright or leaning over a bed table can help
- Supporting patients with pillows, avoiding horse shoe pillows, as patients can slip into the hollow space and compress the lungs
- Supporting arms helps release tension in the shoulders, as does head and neck support
ENVIRONMENT
- A light airy single room if possible, avoiding hot water and humid environments
- Non-restrictive cotton clothing on bed
- A fan with gentle current of air across the face
- The 5th cranial nerve on the face does respond to mechanical and thermal stimuli, so as well as a fan, a cool damp cloth or fine mist spray can be helpful
RELAXATION / ANXIETY REDUCTION
- Touch may or may not be appropriate e.g. gentle stroking on the lower arm or a hand on the shoulder (some patients may find this irritating)
- Massage of hands and feet, aromatherapy oils
- Relaxing music of the patient’s choice
- Visits from family and friends
- A calm approach from the health care professional

