What is an ADVANCE CARE PLAN?
An Advance Care Plan (ACP) is a process of discussion and shared planning for future health care. It is focused on assisting the person to identify personal beliefs, values and priorities and then incorporate these into plans for their future health care. Planning may also involve input from healthcare professionals responsible for the person’s care, along with family, whānau, friends and caregivers. The process is ideally collaborative. 1
ACP relies on the person being competent to share in the planning process and so needs to be considered early in the care of any person for whom the diagnosis of dementia is suspected. A person with advanced dementia will be unable to participate in ACP.2
Suggestions for Implementation in Aged Residential Care Facilities
- Every resident should be offered the opportunity to have an ACP discussion; however the process is voluntary.
- The resident may choose to make decisions about certain aspects of care and not others; this is their choice.
- The resident may choose to have this discussion alone with the health professional, or with several family members/whānau; again, this is their choice.
- The resident should be offered a review of their ACP, or re-offered an initial ACP conversation, at each major change in health status, or at least annually.
The ACP may contain specific Advance Directives (refer to Advance Directive section below).
The InterRAI assessment contains a screening tool, to elicit if the resident has made prior decisions about future care. This tool can be used as an opening for an ACP conversation.
The Advance Care Planning process and documentation helps to inform healthcare decisions if, at some point in the future, the resident’s health changes, healthcare decisions need to be made, and the resident lacks capacity at the time decisions need to be made.
In the case of residents who lack the capacity to make their own informed healthcare decisions, this may mean the resident’s presumed wishes, as articulated by their family. It does not have to be a legalised, formal process, but rather a routine part of the planning of the resident’s care.
What is an Advance Directive?
An Advance Directive is taken to mean a written or oral directive by which the resident makes a choice about possible future treatments that is intended to be effective only when they do not have capacity to make their wishes known (Code of Health and Disability Consumer Rights). This includes Do Not Resuscitate orders.
Right 7(5) of the Code of Health and Disability Consumer Rights states that “Every consumer may use an advance directive in accordance with common law”. Health care providers are obliged to take account of Advance Directives when deciding which services to provide to a resident with diminished capacity.

Suggested Policy/guidelines
The organisation will ensure that every resident is offered the opportunity to engage in Advance Care Planning and to plan for future health care changes with their family and the healthcare team.
Process
1. Initiate the Advance Care Planning discussion.
- All staff i.e RNs and/or ENs, Social Workers, Chaplains and Social Workers will offer the opportunity for an Advance Care Planning discussion to all residents at an appropriate time within the first three months of admission to the facility, or at a change in health status. The ACP information pamphlet will also be offered. This should be incorporated into established processes such as the admission assessment, long-term care plan initiation or review, as well as responding to residents’ requests and cues.
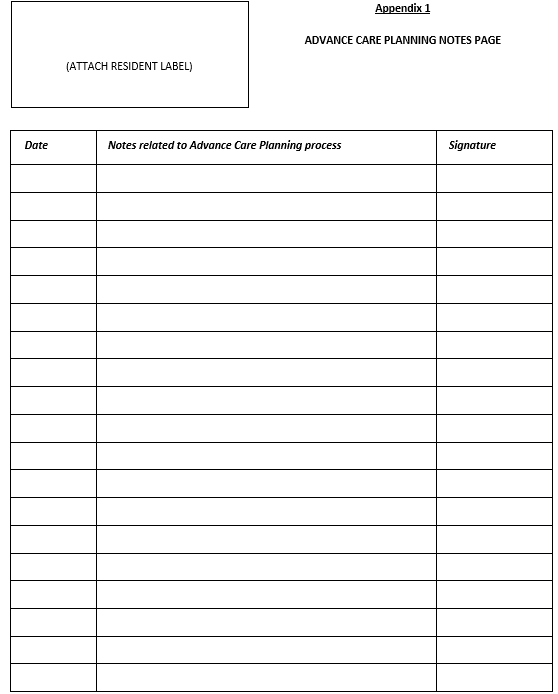
- Advance Care Planning discussions should be initiated by RNs and/or ENs at an appropriate time, taking the conversation(s) as far as their individual skills, and resident/family preference and need, allow. Key points should be recorded on the ACP Progress Notes page (See Appendix One).
- Several Advance Care Planning discussions may be required – remember Advance Care Planning is a process.
- If further discussion is required, and/or it is appropriate to complete a Plan (and the person having the initial conversation(s) does not have the skills or confidence to do so), then a staff member with more training should be contacted. This could be the General Practitioner, Nurse Practitioner, Hospice nurse, or other experienced Registered Nurse.
- Encourage the resident to have their nominated Enduring Power of Attorney for Health and Welfare or family member(s) present (however this is their choice).
- If the resident is unable to make their wishes known, the Advance Care Planning discussion should be offered to the Enduring Power of Attorney for Health and Welfare, or the identified primary contact person if there is no Enduring Power of Attorney (see ‘Advance Care Planning for residents with diminished capacity). Only the resident themselves may make their Advance Directive. If they lack capacity, their EPOA and those who know them can state what they believe the resident would want, if they had capacity. It is then a medical decision, based on this belief, as to which treatments are provided or withheld.
2. Content of discussion
- Review any existing ACP or Advance Directive with resident/family. Screening for the existence of an ACP or Advance Directive is part of the InterRAI assessment, which should be referred to.
- Resident’s values and beliefs; what is important to them in their life.
- Conditions or situations they would find unacceptable.
- What the resident wants us to try and achieve for them overall (e.g. prolonging their life at all costs; to actively treat easily reversible situations but treat more serious situations palliatively; to let nature take its course without trying to prevent or prolong the dying process; make comfort the priority at all costs; and so on).
- Then a more detailed conversation about more specific situations and interventions that relate to their overall preferences, if appropriate, e.g.:
- Preferences with regard to attempted resuscitation
- Preferences with regard to feeding, e.g. spoon-feeding, nasogastric feeding
- Preferences with regard to hospital treatments and investigations
- Any other specific preferences with regard to future care and treatment.
3. Documentation
- An ACP Progress Notes page is to be placed in the front of all resident files. All documentation related to the Advance Care Planning process is to be recorded here. For example whether an ACP conversation has been offered, accepted or declined; key points from any discussion with the resident or family related to future care/treatment preferences that are not documented in an ACP Plan; resident and/or family understanding of current/future healthcare situation; context of a formal ACP conversation and completion of Plan including involvement of resident/family, any associated distress or confusion expressed.
- Ensure all discussions and decisions are clearly documented, avoiding ambiguous statements.
- Ensure any Advance Directive reflects the contents of the ACP, where one exists.
- Ensure the names of all persons involved in the discussion are documented, together with their relationship to the resident, or role (staff member).
- Ensure the ACP is dated correctly.
- The ACP is ideally signed by the resident. If not, the reason should be stated.
4. Liaison with General Practitioner
- Advance Care Planning should be discussed with the General Practitioner at the initial GP visit, and at 3-monthly reviews as appropriate.
- A copy of completed ACP should be forwarded to the General Practitioner. This should be recorded in the ACP Progress Notes page when done. Consider asking the GP to review, discuss (if required) and sign the ACP if it contains statements related to specific treatments or interventions.
- If there is no ACP the General Practitioner should be informed of any significant information the resident or family have shared relating to future care/treatment preferences.
- The General Practitioner should be invited to contribute to an Advance Care Planning review, for example at a 3/12 medical review. Main indicators for an Advance Care Planning review are a change in health status or resident indicates a change in preferences.
- Completed ACP document could be uploaded into the ‘Documents’ section of Medimap so GP has access to a copy and any subsequent reviewed documents.
- A scanned copy of the ACP should also be shared with the hospital so that hospital staff can quickly access it during a hospital admission or in an emergency. Email to acp@midcentraldhb.govt.nz
Future versions of ACPs should also be sent to acp@midcentraldhb.govt.nz
5. Reviewing Advance Care Plans and promoting Advance Care Planning as an on-going process
- Residents should be offered a review of their Advance Care Planning with each change in health status or at least yearly.
- Reviews are to be carried out by an RN with the relevant skills and confidence to have an Advance Care Planning discussion.
- If significant changes are needed, a new form is to be completed; the original is to be kept with the new document.
- Brief additions or minor changes are to be added to the existing form and initialled by the resident/Enduring Power of Attorney and the health professional, and dated.
- As part of ongoing Advance Care Planning, consider asking the General Practitioner to discuss specific treatment options with the resident/family, if necessary.
Advance Care Planning for residents with diminished capacity
In this context a resident with diminished capacity (non-competent resident) is a resident who is unable to make independent decisions about their future care and treatment due to a cognitive impairment which does not allow adequate retention and processing of information.
In this situation, the resident’s Enduring Power of Attorney (or primary contact person if there is no Enduring Power of Attorney) should be offered the opportunity for an Advance Care Planning discussion. The discussion should focus on what the resident may have said to them in the past about their preferences, and what they feel the resident’s preferences would be based on past conversations/knowledge of the resident. NB: family members, including EPOA, cannot legally make future treatment decisions for a resident. Rather, they can provide information that can be used by the doctor/NP to make future medical decisions. For example, “I believe he would not want to be resuscitated” can inform a medical Do Not Resuscitate decision.
The resident should be included in the discussion as far as they are able and wish to. Some residents will have some capacity to indicate values, beliefs and preferences and these should be documented. The extent of resident involvement in the discussion should also be documented.
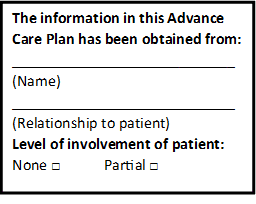
The resident’s preferences, as expressed by their advocate, should be recorded in the ACP, as with residents with sufficient capacity; however it is important that a note is placed on the document indicating that the information has NOT been obtained from the resident, because the legal standing of information obtained from someone other than the resident may be different. The following is a template for a sticker that can be used. This can be printed onto a label sheet or onto plain paper.
Advance Care Planning Document
This should be completed accurately and filed in a consistent place in the resident’s file, usually in the same place as the Advance Directive form and Do Not Resuscitate form; together with the ACP Progress Notes page. Many facilities place these documents in the front of the resident’s file. A copy of the Advance Care Planning document should be provided to the General Practitioner and to the Resident and/or Enduring Power of Attorney if this is the resident’s wish.
A scanned copy of the ACP should also be shared with the hospital so that hospital staff can quickly access it during a hospital admission or in an emergency. Email to acp@midcentraldhb.govt.nz; Future versions of ACPs should also be sent to acp@midcentraldhb.govt.nz
Hospital Admissions
The current Advance Care Plan should always accompany the resident if they are transferred from the facility, and appropriate people notified of the existence of the ACP. For transfers to hospital the Advance Care Planning document and ACP Progress Notes page is included in the transfer documentation and ticked on the yellow envelope.
Residents admitted to hospital will likely be offered a Shared Goals of Care conversation and have their goals for the current admission documented on a Shared Goals of Care form. An Advance Care Plan and related thinking and conversations provide a valuable foundation for developing a person’s goals of care in hospital.
https://www.myacp.org.nz/shared-goals-of-care
If an ACP has previously been shared with the hospital, it should be accessible on the patient’s electronic hospital record.
Using the Advance Care Planning Document
If the resident is capable of making their own care and treatment decisions:
The Advance Care Planning document may be referred to when decisions are being made; however, decisions are made based on the resident’s current preferences, which may differ from the ACP.
For residents with capacity at the time of Advance Care Planning discussion:
If the resident’s health status changes and they are no longer able to express their preferences, the ACP should be consulted in the process of making decisions about the resident’s care and treatment. The medical notes should also be consulted for prior treatment directives; the Enduring Power of Attorney/primary contact person should be consulted and, if necessary, reminded of the resident’s preferences as expressed in the ACP document. The resident’s preferences should be respected unless there is a valid reason, in which case the rationale should be clearly documented in the progress notes. NB Family members cannot override what the resident has previously expressed as their preferences.
For residents not competent at the time of Advance Care Planning discussion:
If the resident’s health status changes and decisions need to be made about the resident’s care and treatment, the ACP document, which would have been completed with the Enduring Power of Attorney/primary contact person, should be consulted. The Enduring Power of Attorney/primary contact person should also be contacted and involved in decision making if possible, and reminded of the content of the ACP if appropriate. If the Enduring Power of Attorney cannot be contacted at the time decisions need to be made, the presumed wishes of the resident, as expressed in the ACP, should be respected unless there is a valid reason not to, in which case the rationale should be clearly documented in the progress notes.
Note that an Enduring Power of Attorney must be invoked before they are able to legally take responsibilities as the resident’s surrogate decision-maker.
An invoked Enduring Power of Attorney must represent the resident’s wishes. They do not have the authority to withhold standard life sustaining treatment, unless the resident has specifically requested this ahead of time while they had capacity.
Following Advance Directives
Remember the resident must have been competent or had appropriate decision-making capacity at the time the Advance Directive was made.
Negative Advance Directives (or anticipatory refusals) indicate a refusal of treatment and, where valid (see below), have the same authority as a valid current refusal of treatment, and therefore such treatment should not be provided, irrespective of whether health care providers consider the treatment would be in the resident’s best interests.
Advance Directives indicating a positive preference for, or consent to receive, a particular treatment do not have the same legal weight as a negative Advance Directive. If the requested treatment is not offered, not available, or would offer no benefit, health care providers are not obliged to provide the treatment; in that case the decision made by an appropriately qualified clinician would take priority. This is a medical decision.
Criteria for a Legally Valid Advance Directive
An Advance Directive is valid (and therefore legally binding) if the resident:
- was competent to make the Advance Directive when it was made,
- made the Advance Directive free from any undue influence,
- was sufficiently informed and had adequate opportunity to receive advice on health care options pertaining to their current and possible future condition(s) at the time they made the Advance Directive, and
- Intended the Advance Directive to apply in the current circumstances.
If there is uncertainty about the validity of the Advance Directive or the applicability of an ACP, then the health care provider concerned should discuss the case with colleagues and/or seek legal advice. Working in the resident’s best interests and according to their ascertainable preferences will help guide challenging decisions.
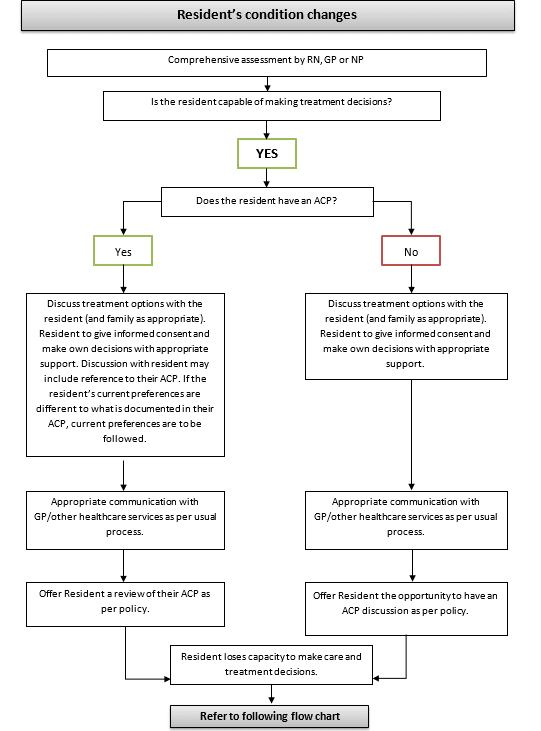
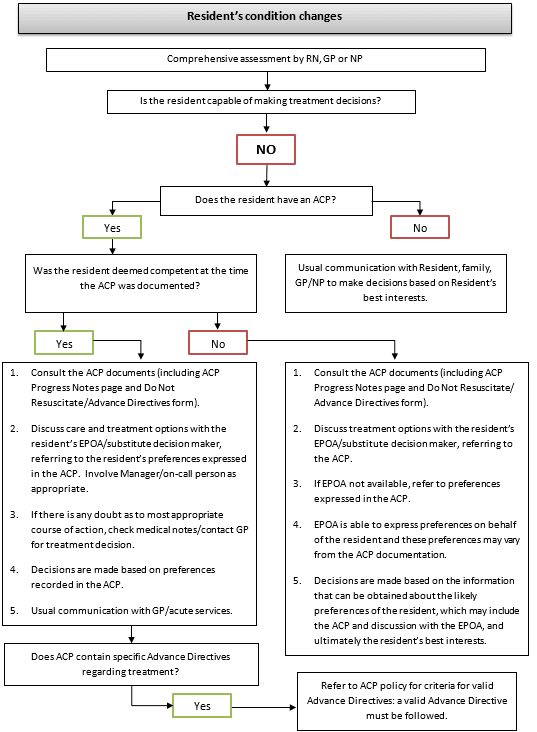
Refer to decision-making flow-charts below.
New Zealand is a multicultural society, and ACP, like all areas of health care, needs to be sufficiently flexible to be culturally appropriate for all individuals in our society. There are differing cultural practices around dying and death that also need to be acknowledged and respected in ACP practices. Health care professionals must be sensitive to different cultural perspectives on how decisions are made and by whom, because there are differing views of autonomy, beliefs and values and how these elements are respected.2
The advance care plan website is an excellent resource to assist individuals, family, whanau and health professionals https://www.myacp.org.nz/
1. The Midcentral District Health Board (MDHB). Palliative Care District Group. (2015). Palliative Care Bereavement Support Guidelines. https://www.arohanuihospice.org.nz/wp-content/uploads/2019/08/Bereavement-Support-Guidelines-2232-Links.pdf
2. Advance Care Planning. https://www.myacp.org.nz/

