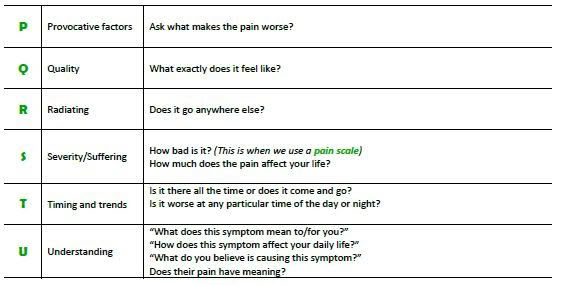
Pain is multifaceted and requires thorough assessment. All residents should have a pain assessment, including location, intensity, and duration in order to determine the cause of pain and appropriate therapy.
Using a reliable standardised assessment scale is useful in addition to performing a clinical assessment, which determines the quality of pain and burden on functioning2. Validated assessment tools include:
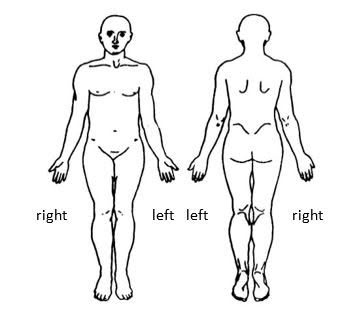
- Body charts
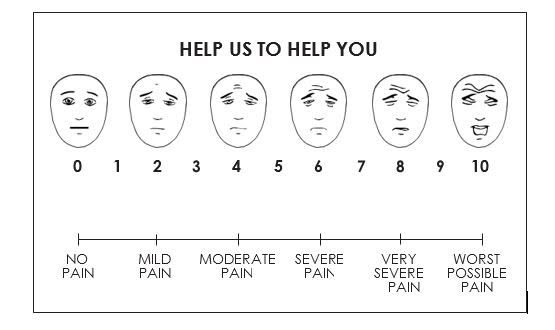
- Neutral facial expression (such as Wong Baker scale)
- Numerical rating scale
- Abbey Pain Scale
The assessment and monitoring of pain and measuring the effectiveness of pain management is essential for effective pain management.1
If a person does not report pain does not mean they do not have pain. Evidence suggests that failing to ask about pain is the most common cause of unrelieved pain and unnecessary suffering.2
In addition, studies have found older people are less likely to report pain or ask for analgesia.3
Dame Cicely Saunders first described Total Pain, which is pain that is not only physical pain, but includes cultural, psychological, emotional, spiritual, and social components as well.3
Physical assessment of pain:
BODY CHARTS
A body chart is a visual tool for mapping location of pain, and marking with pen areas of severe pain, and areas of moderate or mild pain.
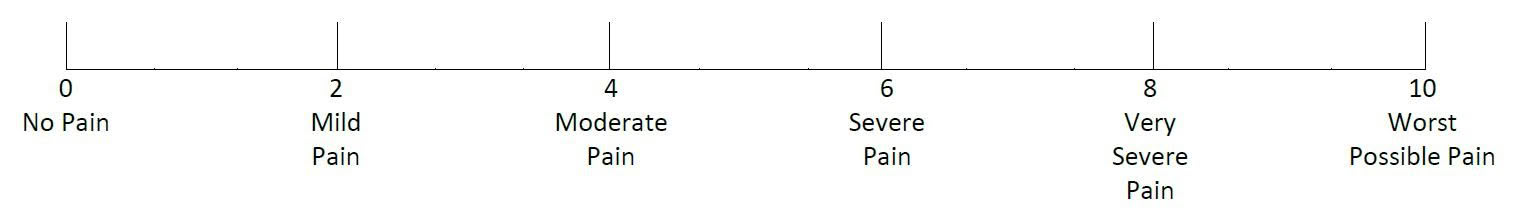
NUMERIC PAIN INTENSITY SCALE
Numerical scales are also useful for rating severity of pain.
THE WONG BAKER PAIN INTENSITY SCALE
This is often used in clinical practice and may be simplified into no pain, moderate pain and severe pain. Ask or indicate to the patient that you require him/her to point to the face which best describes his/her current level of pain/comfort. Assessment must include date, time, and signature of the person making the assessment3.
ABBEY PAIN SCALE
In residents with cognitive impairment and late stage dementia and who cannot verbalise the Abbey Pain Scale4 is an efficient and effective informant-based tool. Assessment includes date, time, and signature of person making the assessment. The tool measures severity of ‘acute pain’, ‘chronic pain’ and ‘acute on chronic pain’4. Each item is leveled on a four point scale for severity (absent: 0; mild: 1; moderate: 2; severe: 3). Item scores are individualised and summed up with a score ranging from 0-18.
| No pain: 0-2 | Mild pain: 3-7 | Moderate: 8-13 | Severe: 14+ |
- Ruder, S. (2010). Seven tools to assist hospice and home care clinicians in pain management at end of life. Home Healthcare Nurse. Retrieved from http://www.hospice.org.nz
- McCaffery, M., & Pasero, C. (1999). Pain. Clinical manual (2nd ed.). St. Louis, MO: Mosby.
- Australian National Health and Research Council. (2006). Guidelines for a Palliative Approach in Residential Aged Care. Retrieved from https://www.nhmrc.gov.au/_files_nhmrc/file/guidelines/pc29_guidelines_for_a_palliative_approach_in_residential_aged_care_150609_0.pdf
- Abbey, J; De Bellis, A; Piller, N; Esterman, A; Giles, L; parker, D and Lowcay, B. Funded by the JH & JD Gunn Medical Research Foundation 1998-2002.

