When a palliative approach is taken medicine review is required
Reviewing medicine includes:
- discontinuing non-essential medicines
- starting medicines to improve comfort (eg, symptom management for pain, agitation, anxiety, nausea, vomiting, respiratory tract secretions), including anticipatory prescribing of palliative medicines
- reviewing administration routes (eg, subcutaneous when there are swallowing difficulties):
- do not stop medicines that enhance comfort because the patient cannot swallow (eg, pain medicine for arthritis)1.
The use of 'as needed' medications is a standard aspect of patient management in aged residential care settings. It is a practice in which doctors or nurse practitioners and nurses are interdependent. Doctors or nurse practitioners prescribe the medications and nurses make the clinical decisions to administer them. This requires appropriate assessment and clinical decision-making by the registered nurse.
PRN medications may only be used in a specific situation (e.g. intermittent chest pain, constipation, pain, nausea or vomiting, agitation or restlessness or for upper respiratory tract secretions).
PRN medicines
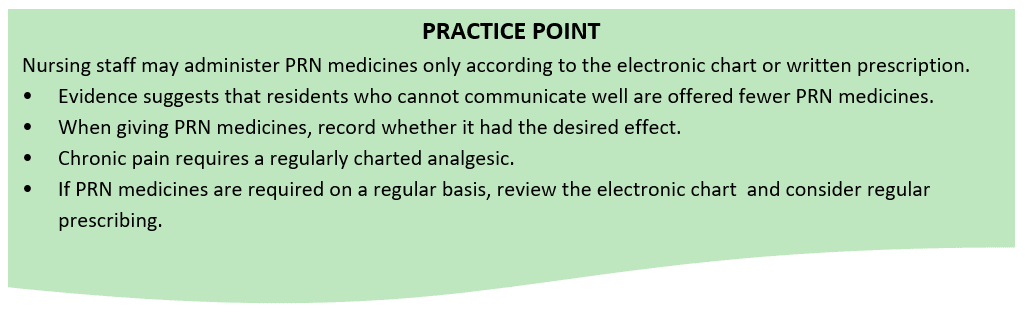
Prescriber orders for all PRN medicines must have:
- specific target symptoms
- instruction(s) for the PRN medicine use
- an indication of the frequency and dose range
- the rationale for using the PRN medicine.
END OF LIFE CARE
Anticipatory Prescribing and PRN medications use for end of life
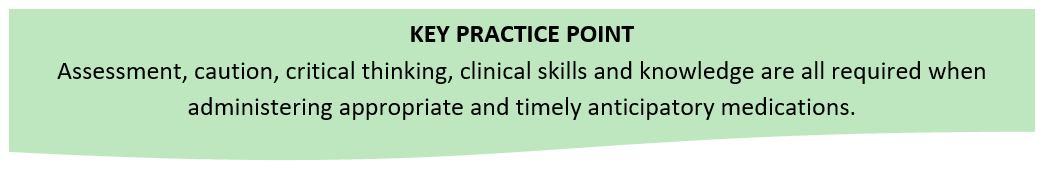
When a person is entering last days of life a medication is often charted before it is needed in anticipation of managing symptoms such as pain, nausea, agitation, respiratory secretions and breathlessness. Nurses have a central role in assessing a dying person’s need for symptom management and activating the anticipatory prescriptions2.
Critical factors:
- Assessment: Identify the health need and potential cause/contributing factors (nursing diagnosis) this will inform the selection of the right medication, the right dose and the right route. For example - give a nauseated person an antiemetic by a subcutaneous (s/c) route if available and charted rather per oral. If not charted and needed, request it be charted subcutaneously. It is the clinical responsibility of registered nurses to carry out first hand assessments before administering s/c prn medication.
- Evaluate and document your findings, including the effects of PRN medications (efficacy). Your rationale should always be evident. Review your facility procedure for “activating Anticipatory Medication” it may require sign off and assessment by two RN staff.
Remember:
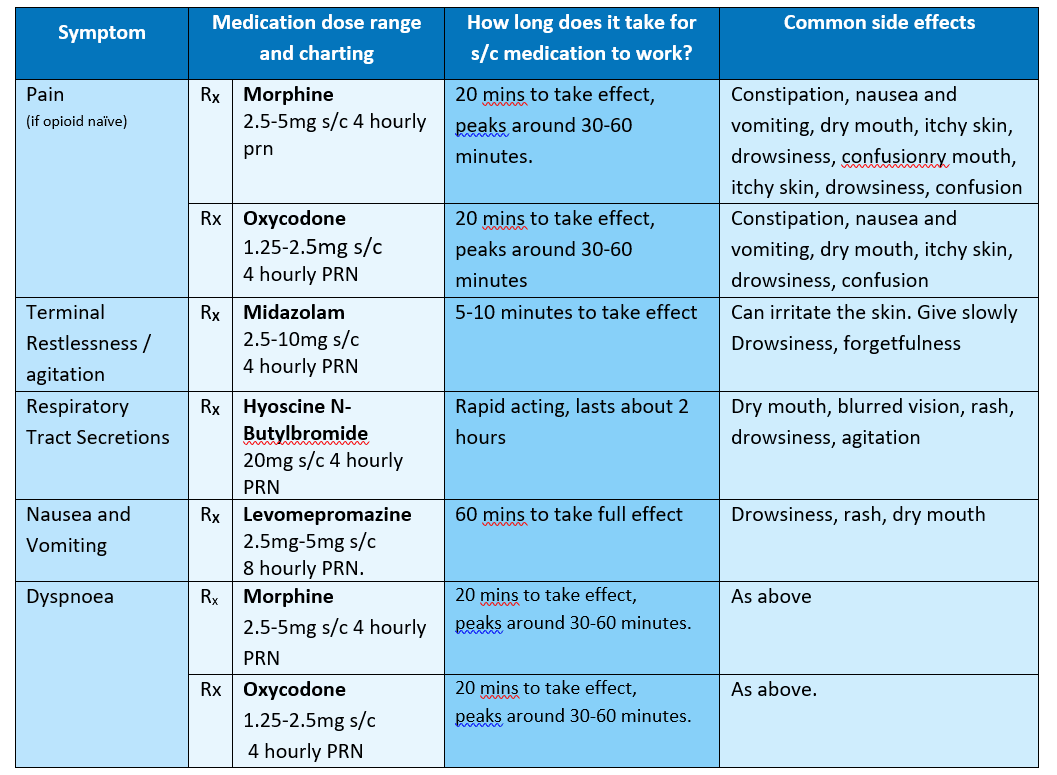
- Give the lowest dose in the range the first time the medication is administered and evaluate efficacy. For example: 2.5 - 5mgs q 4hly. Give 2.5mgs and review in 30 minutes. If inadequate, an additional 2.5mgs can be given as long as the maximum of 5mgs in 4 hours is not exceeded.
- Utilise the right medication for the right reason. Analgesic for pain, antiemetics for nausea and vomiting, anxiolytics for anxiety and restlessness. Note the only clinical indications for morphine are pain and breathlessness. For breathlessness usually only a small dose eg. 2.5-5mgs is given. Morphine is not clinically indicated for agitation and/or restlessness unless this is caused by pain.
- PRN medications and continuous subcutaneous infusions. PRN medications can and should be used with subcutaneous infusions for symptom management. If starting a syringe driver and the person is symptomatic, administer the appropriate PRN medication for the symptom and then get the syringe driver established – it will take an estimated four hours for most of the drugs administered via syringe driver to reach a therapeutic level. Hence use the PRNs to control symptoms first.
The following medications and dose guidelines are recommended for symptom management in the last days of life.
Indications for initiating a syringe driver (SD):
- A syringe driver is indicated if the patient has difficulty swallowing, poor absorption of oral medicines, multiple symptoms, or if their symptoms are not controlled by ongoing subcut PRN medications (i.e. more than 3 doses of subcut PRN medications in 24 hours).
- If a resident is already on regular opioids, the dose range may be different from above.
- Refer to Arohanui Hospice for Syringe Driver Management if required.
- PRN medication can and should be used with a syringe driver for symptom management.
1 Ministry of Health (2011). Medicines Care Guides for Residential Aged Care Wellington; Ministry of Health.
2 Wilson, E., Morbey, H., Brown, J., Payne, S., Seale, C., & Seymour, J., (2015). Administering anticipatory medications in end of life care: a qualitative study of nursing practice in the community and in nursing homes. Palliative Medicine. 29(1) 60-70.

